If you are experiencing lower back pain when standing, you are one of 84% of the world’s adults who are faced with this health issue at some point in their lives [1]. It is the second most common reason people visit a doctor after upper respiratory infections [2] and the leading cause of disability and loss of productivity worldwide [1].
However, due to the large number of complaints, referral times can be very long so the NHS can’t always help you with your back pain [3]. You may be asked to wait for up to 18 weeks to be seen by a specialist [4]. However, self-paying patients and those who are privately insured can opt for an often same day consultation with one of the experienced pain management consultants in a private hospital, such as the Harley Street Specialist Hospital.
The good news is, however, that your lower back pain while standing is rarely serious. In approximately 97% of cases, it is mechanical in nature, caused by muscle strain, a trapped nerve or a herniated disc in your spine. However, should you be one of the 20% of patients whose pain worsens or does not resolve within 6 weeks [1], it is recommended that you see a healthcare provider.
Keep reading this article to learn all you need to know about:
- Why standing up causes lower back pain
- How to tell what may be causing your lower back pain when standing
- Ways to treat the pain in your lower back
- When you need to worry about your back pain when standing
Table of Contents
- Why does my lower back hurt when standing?
- Is your lower back pain when standing caused by your muscles, nerves or systemic illness?
- Tips to get relief at home for lower back pain when standing
- What medical treatment options are there for lower back pain?
- When should I be worried about lower back pain?
- Are you looking for treatment for your lower back pain when standing?
Why does my lower back hurt when standing?
The most common reason why your lower back might hurt more when standing for a prolonged time is that due to gravity and the need to support your body weight, your spine and back muscles are under increased pressure when in an upright position [5]. In fact, one study found that simply standing for 2 hours induced temporary lower back pain in 50% of its healthy participants, due to back muscle fatigue [6].
This proportion can increase significantly if you are routinely spending a lot of time on your feet and/or you have spinal disorders or other relevant medical problems. Here are some of the most common reasons why your lower back hurts when you are standing:
1. Muscle strain or ligament sprain

Approximately 70% of mechanical lower back pain when standing is caused by straining the muscles of your lower back or spraining a ligament. This can happen from trauma, excessive effort, sudden movements or maintaining an uncomfortable position for too long. It can cause the following symptoms [7]:
- Lower back pain which gets worse with movement
- Lower back stiffness
- Discomfort when maintaining normal posture
- Muscle spasms with activity or at rest
Here are the most common ways in which you can strain a muscle or sprain a ligament in your lower back:
Injury
Taking a fall or hitting your back forcefully can put pressure on your muscles and ligaments, stretching them too far.

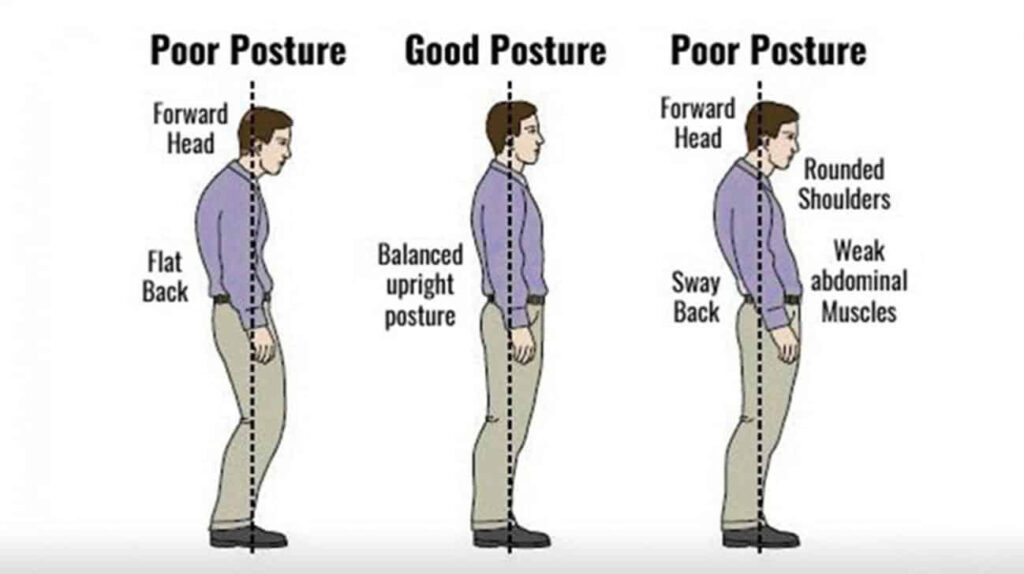
Poor posture
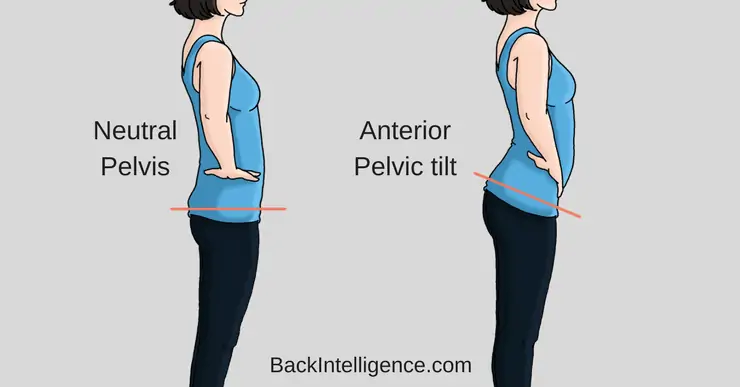
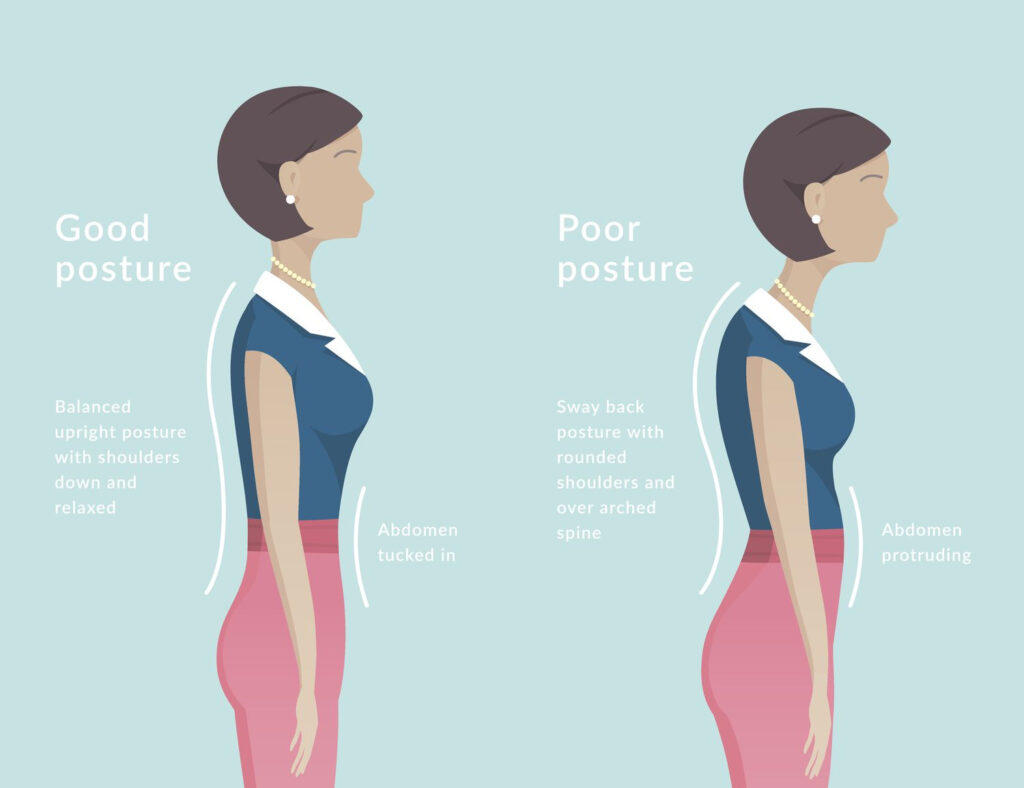
Unhealthy postures, where your spine is not aligned and your balance centre is offset, can put strain on your lower back muscles when you are standing up. These include [8]:
- Standing or walking with your hips tilted forward
- Slouching (standing with your shoulders pushed forward and your back rounded)
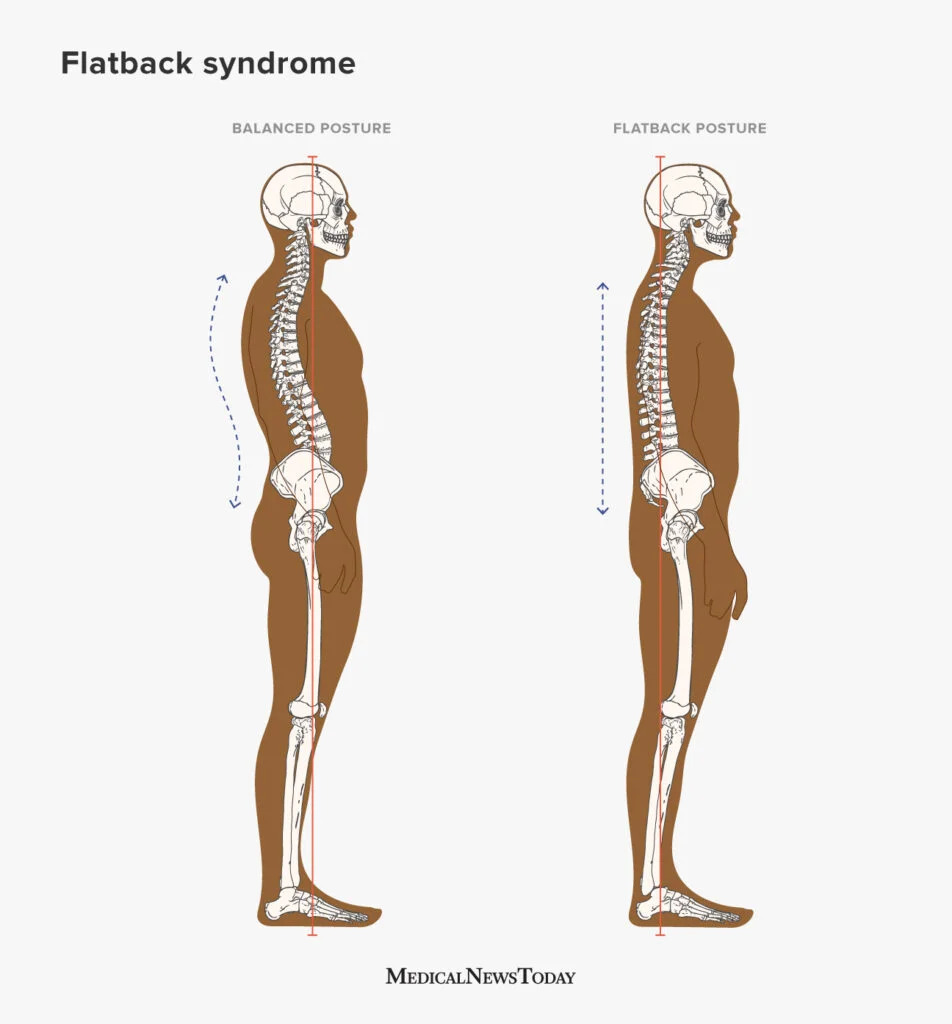
- Flat back (when your spine loses its natural curvature, becoming flatter in time)
Lifting heavy objects
Lifting with your back, or stooping to lift a heavy object can put significant strain on your back muscles and ligaments, which can cause pain when standing or moving [19].

A weak core – not exercising your core muscles sufficiently can lead to weak back muscles, which will strain more easily with effort or sudden movement.
2. Your discs getting worn out
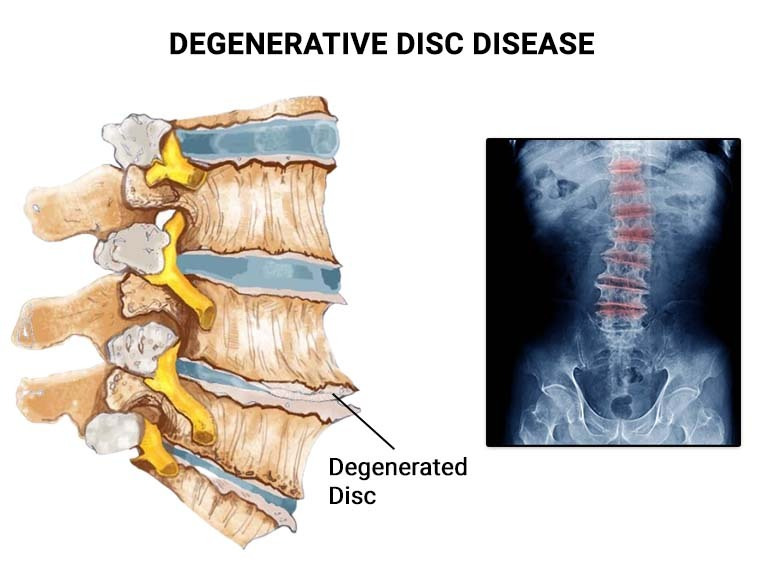
As you advance in age, wear and tear on your spine can cause the discs between your vertebrae to get worn out. This can cause chronic lower back pain, with symptoms such as [9]:
- Pain that is worse when standing for long periods of time or sitting, but can improve when walking or running.
- The pain increases when bending or twisting.
- Periods of intense lower back pain that come and go (lasting from a few days to several months).
- The pain may radiate to the buttocks and thighs.
- Numbness and tingling in the legs.
- Weakness in the leg muscles.
Since your discs act as a sort of cushion between your vertebrae, which absorb shock and prevent friction, when they become worn out, your vertebrae will experience more shock and may end up rubbing against each other. Standing for longer periods of time makes your vertebrae become even more compressed, with worn out discs as a buffer, making it easier to pinch and press on your nerves.
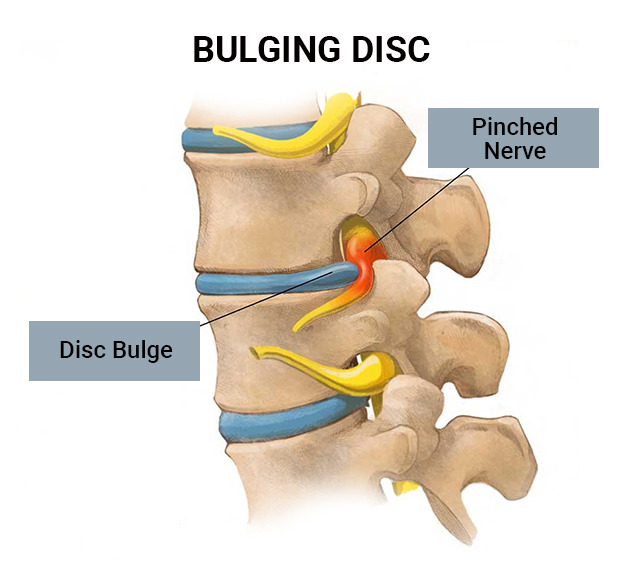
3. A slipped disc in your spine
Sometimes, because of trauma, heavy lifting or sudden movements, one of the discs in your vertebrae can slip out of place and pinch a nerve. The same can happen when a bone moves and traps a nerve. When this occurs in your lower back, you may get sciatica. This is the name for an array of neurological symptoms, such as [10] [11]:
- One sided sharp pain in your lower back which radiates to your buttock
- Shooting pain in your leg
- Numbness or tingling in your affected buttock and leg
- Weakness in the affected leg
- Pain that worsens with prolonged standing or sitting, as well as with movement of the affected area
Since pressure on your discs increases when you are in an upright position, your slipped disc can protrude more when you are standing for longer and increase your symptoms.
4. A narrowing in your spinal canal
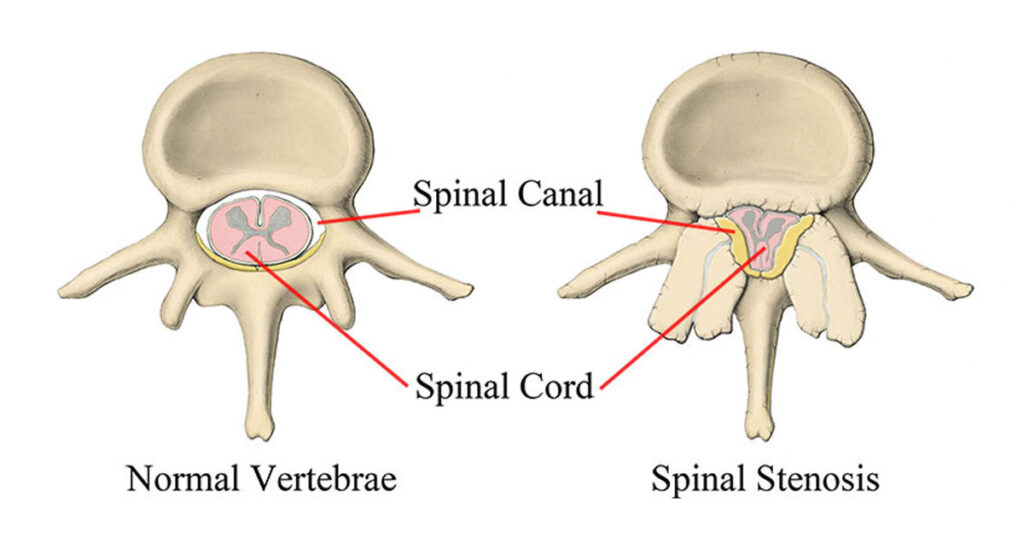
A slipped disc is not the only thing that can give you sciatica, so can a narrowing of your spinal canal, known as spinal stenosis. This can happen due to a number of conditions, such as injury, arthritis, past surgery or bone disease [12].
This condition causes similar symptoms as those of a slipped disc, but in some cases, neurological symptoms can be more severe, such as difficulty walking or maintaining your balance.
Standing in an upright position worsens the symptoms of spinal stenosis, as the vertebrae get compressed, adding more pressure to the nerves [13], while bending over alleviates pain [2].
5. A compression fracture in your spine
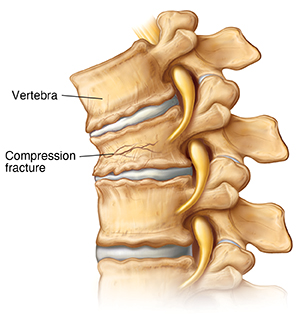
If the bones in your spine get brittle, often due to conditions such as osteoporosis, they can become compressed under the weight of your body, producing severe pain and making you decrease a few centimetres in height. This condition is often encountered in patients over the age of 50 and it affects women more than men. It can be encountered in 40% of postmenopausal women by the time they reach 80 [14]. Its symptoms include:
- Sudden onset of lower back pain
- Pain that is worse when standing or walking and improves when lying down
- Limited mobility in your back
- Height loss
Since this issue occurs as a result of compression, the weight of your body pressing down on your fractured disk is the highest when you are standing upright.
6. Premenstrual syndrome

Data shows that as many as 90% of all menstruating women have experienced some premenstrual symptoms during their lifetime and that many of them fit the diagnosis criteria for premenstrual syndrome (PMS) [15]. One of the common symptoms in PMS is dull lower back pain in females, which can be made worse by standing or walking for long periods of time or by increased effort.
One study conducted on 384 young women has revealed that 53% of them fit the criteria for PMS. Out of those who were experiencing this syndrome, over 77% reported lower back pain (62% mild or moderate and 15% severe in intensity) [15].
So, if you notice cramps or dull pain in your lower back when standing in the days that lead up to your menstruation, it may be due to PMS.
7. A non-spinal systemic disease

Rarely, in about 2% of cases, lower back pain can be the result of an illness which has nothing to do with your spine, but the pain from a diseased organ radiating to your lower back.
Such conditions include [2]:
- Pelvic organ disease
- Kidney disease
- Digestive system disease
- Very rarely, aortic aneurysm (this is usually accompanied by sudden, severe abdominal pain)
Since an upright position causes increased pressure on the organs in your abdomen and pelvis, standing for a long time can increase pain from an injured or inflamed organ. So if you have ruled out any muscular or spinal causes for your lower back pain when standing and also have other health symptoms (e.g. abdominal pain, nausea, fatigue, fever), you may want to ask your GP if it would help to be tested for systemic illness.
8. Spinal tumours

If you are worried about cancer in your spine, rest assured that while not impossible, this is a very rare occurrence. Spinal cancers are only diagnosed in only less than 0.1% of people who see a doctor for lower back pain [1].
Non-cancerous tumours can also grow in your lower spine, putting pressure on your nerves and causing pain and neurological symptoms.
The symptoms of spinal tumours can be mostly the same as those of a pinched nerve caused by a slipped or fractured disk. And they can worsen when you are in an upright – standing or sitting – position, as pressure on your trapped nerve is increased.
However, you may also be experiencing severe neurological symptoms such as paralysis, numbness in your genital area and/or suddenly becoming unable to control urination or bowel movements. While these symptoms may not always be caused by cancer, they do warrant calling emergency services.
Is your lower back pain when standing caused by your muscles, nerves or systemic illness?
There is no way to know for sure what causes your lower back pain without thorough medical testing, such as diagnostic imaging. However, there are some unique symptoms of each of these types of pain that you can use to get some idea about the cause of your discomfort:
Symptoms of lower back pain by condition [16]
| Muscle strain/joint sprain pain | Nerve pain | Systemic illness pain |
|---|---|---|
| • Is usually aching or throbbing. | • Is usually sharp or burning. | • Is often deeper and duller than muscle or nerve pain. |
| • Is made worse by certain movements (e.g. standing, bending, twisting, lifting). | • Is worse when standing or sitting. | • It can radiate to other places in your back or abdomen, but rarely to your limbs. |
| • It can manifest as tenderness to the touch. | • Is usually accompanied by tingling and numbness in your buttocks and leg. | • It is not normally accompanied by tingling, numbness or altered temperature sensitivity. |
| • It can be accompanied by stiffness. | • It can alter your sensitivity to hot and cold. | • It does not normally worsen with movement. |
| • It does not normally cause tingling or numbness in your limbs. | • It doesn’t usually manifest with tenderness to the touch. | • It is often accompanied by other symptoms, such as nausea, fatigue, abdominal pain or fever. |
| • It can radiate to your buttock, but usually not to your leg. | • It can worsen with certain movements. | • It does not normally manifest with tenderness to the touch, but the pain can worsen when the affected area is pressed or tapped. |
| • It can be alleviated with a massage or hot/cold compress. | • It tends to last longer than muscle pain (e.g. a few weeks to a few months). | • Usually subsides once the underlying cause is resolved. |
| • It is often short term (a few days to a few weeks) | • It is not usually accompanied by symptoms such as nausea, fatigue, abdominal pain or fever. | |
| • It is not usually accompanied by other symptoms, such as nausea, fatigue, abdominal pain or fever. |
Tips to get relief at home for lower back pain when standing
While the best way to get relief for your lower back pain when standing depends on the condition which caused it, there are some things you can do which are generally helpful in most types of lower back pain:
- Do some light exercise and stretching – some light yoga or pilates, or even a slow walk can often do you good and in some cases, they can temporarily provide immediate relief for sciatica pain. However, if you see that your lower back pain gets worse with running or other more intense exercises, avoid overexerting yourself.

Avoid standing (and sitting) for prolonged amounts of time – the upright position puts pressure on your muscles and discs and can make your symptoms worse. Take breaks during the day to lie down on your back and rest.

- Improve your standing posture – standing straight, with your spine properly aligned and your shoulders in line with your chest and pelvis, can relieve pain when standing.
- Wear comfortable shoes – wearing high heels or uncomfortable shoes which affect the way you walk can lead to increased stress on your lower back and spine.
- Lose some weight – lowering your body mass can help take some pressure off your muscles, joints and spine and relieve some of your pain. Even one month of a low-calorie diet can yield good results [18].

Get a relaxing massage – a deep tissue massage can do wonders for your muscles and if you use the right massage techniques for sciatica pain relief before bed, it can even help you sleep better with sciatica [18].

- Use hot or cold compresses to reduce pain and inflammation [10] – whether you have a muscle strain or a pinched nerve, applying both warmth and cold can be soothing and relieve some of your symptoms.

What medical treatment options are there for lower back pain?

If your lower back pain when standing doesn’t subside in a few weeks, it is a good idea to see your healthcare provider, to rule out a more serious condition and get a referral for the treatment you need. Depending on the cause and severity of your condition, this treatment may include [1][2]:
- Physiotherapy
- Spinal manipulation and massage therapy
- Pain medication
- Certain types of injections for back pain (e.g. steroid injections)
- Spinal surgery
When should I be worried about lower back pain?

In most cases, lower back pain is not caused by any serious condition and will heal without treatment in a few days or weeks. However, there are also situations when you need to contact your healthcare provider [10]:
Contact your GP at your earliest convenience if:
- You don’t see signs of sciatica improvement after 6 weeks.
- Your pain or neurological symptoms are gradually getting worse.
- You can see swelling or bruising on your lower back with no injury.
- You develop other mild health symptoms, such as fatigue, mild digestive symptoms, and low-intensity headaches.
Contact emergency services as soon as possible if:
- You have sciatica on both sides of your body (bilateral sciatica).
- You can no longer feel your legs.
- Your sciatica is so bad you can’t walk or move your legs.
- You can’t move with sudden, severe lower back pain (especially if it is accompanied by abdominal pain).
- You have significant difficulties standing or walking.
- You are experiencing numbness around your genital area and/or anus.
- You are suddenly no longer able to control your urination or bowel movement.
- You suddenly no longer feel the need to urinate or have bowel movements.
- You are also experiencing other severe symptoms, such as high fever, severe. headaches or abdominal pain, or vomiting.
Are you looking for treatment for your lower back pain when standing?
Living with pain can be difficult and taxing on every aspect of your life. So if you have decided you can’t spend one more day with lower back pain when standing, we are here to help you. Book an appointment now with our team of specialists and we will use modern diagnostic imaging tools to get to the root of your condition in the shortest amount of time.
Once diagnosed, we will provide you with the best, evidence-based treatments for the back and spine, from private physiotherapy to steroid injections and radiofrequency treatments. In the event that you need surgery, you will be in the most capable hands and benefit from state-of-the-art equipment, which increases your chances of an excellent outcome, such as curing your sciatica permanently.




