Epidural steroid injections are used to deliver corticosteroid medication into your spine, relieving pain from chronic or debilitating conditions like sciatica and other nerve compression problems.
Generally, epidural steroid injections are a safe way to manage severe or chronic back pain. Research indicates a steroid injection success rate of 50% to 84%, depending on the condition being treated [1].
But perhaps unsurprisingly, there are certain risks associated with epidural steroid injections. In this article exploring the dark side of epidural steroid injections, we’ll discuss the potential risks, complications, and side effects of spinal steroid injections, and what you can do to minimise these.
Table of Contents
What is an epidural steroid injection?
An epidural steroid injection involves inserting a needle into the epidural space of your spine and injecting a steroid such as cortisone. A local anaesthetic is also given to numb and reduce pain in the area for a few hours after the procedure.

Complications can arise when the needle and/or steroid is inserted or administered incorrectly. Watch this video to see how an epidural steroid injection is performed:
Epidural steroid injections can be used to treat conditions including:
- Sciatica — A painful condition caused by compression of the sciatic nerve (usually by a herniated disc).
- Trapped nerves — Other types of spinal nerve compression can also be treated with epidural steroid injections.
- Localised low back pain — Non-specific back pain that affects the lumbar (lower) region of the spine. It may have multiple causes.
Can steroid injections do more harm than good?
Epidural steroid injections have a proven track record of providing safe and effective pain relief to patients with sudden or severe back pain, especially in the short- to medium-term [1-3].
For most patients — particularly those with high levels of inflammation around the spine — lumbar epidural steroid injections are very safe [1]. But in rare cases, they may actually cause more problems than they solve.
Can an epidural injection go wrong?
An epidural steroid injection can have serious consequences if it’s not administered correctly, or the patient isn’t suitable for the procedure.
Known adverse effects of epidural steroid injections include:
- Neurological symptoms, including an inability to swallow, vertigo, and worsening neck pain [4-5].
- Epidural headache, an intense headache that can happen if medication leaks out of the epidural region into the surrounding area.
- Infection (a known risk of any injection or semi-invasive procedure).
- Haematoma (excessive bruising around the injection site).
What’s the worst that can happen with an epidural?
The dark side of epidural injections is that, in extremely rare cases, they can result in convulsions, serious infection, permanent nerve damage, severe breathing difficulties, and even death.
Permanent nerve damage results from spinal cord damage or severe infection caused by an epidural injection. It can lead to permanent loss of feeling (paralysis or paraplegia) in your legs.
Estimates show that permanent harm occurs in less than 1 in 50,500 (0.002%) spinal or epidural injections [5]. Paraplegia or death happens in less than 1 in 141,500 (0.0007%) cases. So the risk of the worst happening is extremely low.
What happens if a steroid injection hits a nerve?
An epidural steroid injection hitting a nerve isn’t always a cause for concern. It may trigger a brief tingling sensation, pins and needles, or a mild shooting pain. None of these signs necessarily mean the nerve is damaged, but the needle may need to be repositioned.
If the needle hits a nerve and isn’t repositioned, it can lead to further problems. So let your anaesthetist know if you experience any unusual sensations following an epidural injection.
5 reasons not to get an epidural steroid injection
For most people, there’s only a tiny risk of permanent damage resulting from an epidural steroid injection. So if this treatment is recommended or prescribed by your medical practitioner, there are very few reasons to turn it down.
However, in some cases you may decide against getting an epidural steroid injection:
- You feel the risks outweigh the benefits.
- Your doctor says the risks outweigh the benefits.
- You’ve been advised not to have an epidural steroid injection due to your medical history or current health conditions.
- You’ve already had a steroid injection within the last three months, or four in the last year.
- You have a weakened immune system.
Make sure to discuss the risks and benefits of an epidural steroid injection with your doctor. They can help you decide whether this is the right course of action for your condition.
What is the black box warning for epidural steroid injections?
In 2014, the US Food and Drug Administration issued a warning to patients considering epidural steroid injections [6]:
“The U.S. Food and Drug Administration (FDA) is warning that injection of corticosteroids into the epidural space of the spine may result in rare but serious adverse events, including loss of vision, stroke, paralysis, and death. The injections are given to treat neck and back pain, and radiating pain in the arms and legs.”
There has been some pushback from the medical community since this black box warning was issued [7]. One review assessed certain inaccuracies in the warning, referencing alternate techniques and risk factors when performing certain types of injections for back pain to improve safety [7].
The American Society of Anaesthesiologists issued a response to the FDA stating [8]:
“The message inaccurately groups all epidural steroid injections into one broad warning, but the critical distinctions between the routes of administration and formulations of steroids represent the difference between safe and effective use of epidural steroid injections and unsafe use associated with catastrophic injuries.
“We strongly recommend that the Warning be retracted and replaced with one that accurately represents the risks associated with epidural steroid injections used to manage painful spinal conditions.”
As with all medical procedures, you should discuss the risks and benefits with your doctor beforehand. But it’s also important to note that this black box warning has been challenged by several professionals in the field.
How to reduce the risks of epidural steroid injections
Epidural steroid injections do carry some risks. But in the vast majority of cases, they’ll improve your symptoms and leave you feeling much better than you did before your procedure.
To minimise the chance of things going wrong, here are four ways to reduce the risks of an epidural steroid injection.
1. Ask your anaesthetist about the procedure
Knowledge is power. Ask your doctor to tell you exactly what will happen in the procedure so you know what to expect. Take this opportunity to ask any questions you have about the risks.
Know the signs that may require the needle to be repositioned, such as tingling, shooting pains, or pins and needles on receiving the epidural.
2. Work with an experienced medical team
Experienced anaesthetists are more likely to have the skill, knowledge, and experience to correctly perform your procedure. Choosing a private medical team means you can get to know your practitioners in advance, so you feel completely comfortable with the team performing your epidural.
In our specialist pain management unit, we work with the largest pool of pain management consultants in the UK, helping you find the right team to meet your goals. Book an appointment with the Harley Street Specialist Hospital team to meet an epidural specialist who can talk through the risks and benefits of this procedure with you.
3. Know about the risks of different spinal injections
Transforaminal epidural steroid injections (TFESI) are more likely to result in complications than interlaminar (ILESI) and caudal injections [8].
In TFESI, the needle injects the medication into an opening at the side of the spine. In ILESI, the steroid is injected between the vertebral layers. Caudal epidurals are delivered to the epidural space via the base of the spine.
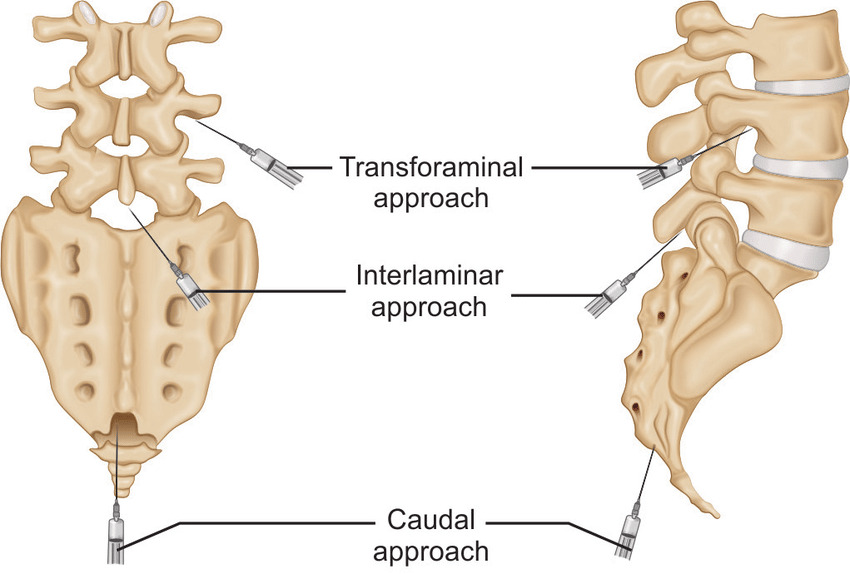
Caudal epidurals are considered the safest approach, but transforaminal injections allow a smaller dose to deliver effective pain relief [9]. Your doctor will talk through the pros and cons of each approach with you.
4. Rest after your procedure
Steroids need to stay in the targeted area for as long as possible to provide effective pain relief, but also to reduce the risk of systemic absorption into the bloodstream. Systemic absorption can lead to problems including loss of bone density, infection, and high blood sugar [10]. Getting enough rest may also prolong how long your epidural injection lasts for back pain.
Take it easy for at least a few days after your procedure, or longer if your doctor recommends it. Find out more about resting after a cortisone injection.





